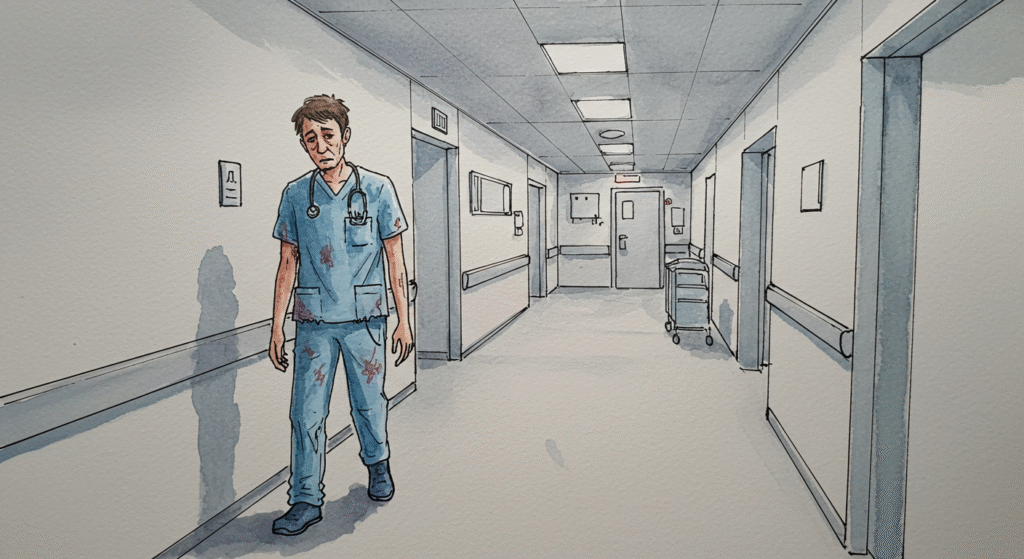
Healthcare workers are some of the most dedicated professionals in the world. They show up day after day—often during nights, weekends, and holidays—to care for patients when they are at their most vulnerable. But behind the professionalism, compassion, and clinical expertise lies a growing crisis: burnout.
Burnout among healthcare workers has been on the rise for years, and the COVID-19 pandemic amplified an already urgent issue. According to multiple studies, healthcare professionals are at significantly higher risk for emotional exhaustion, depersonalization, and even leaving the profession entirely compared to other industries. Self-care is no longer a luxury for those in healthcare—it’s a necessity.
This article explores why self-care is critical for healthcare workers, what it really means in practice, and how it can benefit both providers and patients.
Understanding Burnout in Healthcare
Burnout is more than just being tired after a long shift. The World Health Organization defines it as an occupational phenomenon characterized by three components:
- Emotional Exhaustion – Feeling drained, overwhelmed, and unable to recover between shifts.
- Depersonalization – Developing a sense of detachment from patients, coworkers, or even oneself.
- Reduced Personal Accomplishment – Feeling ineffective or questioning one’s purpose in the work.
Healthcare workers often face unique stressors that can accelerate burnout, including:
- Long and irregular hours that disrupt sleep and work-life balance.
- Emotional labor from witnessing suffering, loss, and trauma daily.
- Administrative burdens like documentation, compliance requirements, and productivity quotas.
- Staffing shortages that increase workloads and reduce support.
Left unaddressed, burnout can lead to mental health struggles such as depression, anxiety, substance use, or even suicidal thoughts. It also affects patient care, increasing the likelihood of medical errors, lower patient satisfaction scores, and higher turnover rates.
Why Self-Care Matters for Healthcare Workers
Self-care is not selfish—it is survival. For healthcare workers, practicing self-care can help:
- Restore energy levels and prevent chronic exhaustion.
- Preserve compassion so they can continue to engage empathetically with patients.
- Maintain professional competence by reducing cognitive fatigue that can impair judgment.
- Model healthy behaviors for patients who look to them as examples of well-being.
Most importantly, self-care allows healthcare professionals to sustain their careers over time rather than burning out and leaving the workforce altogether.
Common Misconceptions About Self-Care
One of the biggest barriers to self-care in healthcare is mindset. Many clinicians have been trained to prioritize others’ needs above their own. Some believe that needing rest or support shows weakness. Others think self-care has to be expensive, time-consuming, or elaborate—like taking spa trips or week-long vacations.
In reality, self-care can be simple, affordable, and practical. It’s about consistent, small actions that protect your mental, emotional, and physical well-being.
Practical Self-Care Strategies for Healthcare Workers
1. Prioritize Sleep
Sleep is the foundation of resilience. Working night shifts or rotating schedules can make sleep hygiene challenging, but it’s still crucial to protect rest as much as possible.
- Establish a pre-sleep routine to signal your body that it’s time to wind down.
- Use blackout curtains and white noise machines to create a restful environment.
- Limit caffeine several hours before bedtime.
Even incremental improvements in sleep can dramatically improve mood, memory, and decision-making.
2. Nourish Your Body
Busy shifts can make skipping meals or relying on vending machine snacks tempting, but good nutrition fuels better energy and focus.
- Pack balanced meals and snacks when possible.
- Stay hydrated by keeping a refillable water bottle nearby.
- Limit excessive sugar and processed foods that can cause energy crashes.
When the body is fueled properly, mental resilience is easier to sustain.
3. Move Your Body
Exercise doesn’t have to mean hours at the gym. Even short bursts of movement can reduce stress and boost endorphins.
- Take the stairs when possible.
- Go for a 10-minute walk on your break.
- Try gentle stretching or yoga before or after shifts.
Regular physical activity improves sleep, mood, and cardiovascular health—key components of long-term well-being.
4. Set Emotional Boundaries
Compassion fatigue is real, and learning to set boundaries is vital.
- Allow yourself to take breaks, both physically and emotionally.
- Debrief with trusted colleagues after difficult cases.
- Remember that caring for patients does not require absorbing their pain.
Healthy boundaries allow healthcare workers to stay empathetic without depleting themselves completely.
5. Stay Connected
Support systems are one of the strongest predictors of resilience.
- Build relationships with coworkers who understand the unique challenges of healthcare.
- Stay in touch with family and friends outside of work to maintain perspective.
- Seek mentorship or peer support groups when struggling.
Social connection helps counter feelings of isolation and strengthens emotional reserves.
6. Practice Mindfulness and Stress Management
Mindfulness doesn’t have to be complicated—it can be as simple as taking a few deep breaths before walking into a patient’s room.
- Try guided meditation apps for short daily sessions.
- Use deep breathing exercises to lower stress during chaotic moments.
- Keep a gratitude journal to focus on positive moments from your shift.
These small habits can reduce anxiety, improve focus, and help healthcare workers remain present in the moment.
7. Seek Professional Help When Needed
There is no shame in needing extra support. Healthcare workers are at higher risk for mental health challenges, but stigma still prevents many from seeking care.
- Consider talking to a therapist, counselor, or peer support specialist.
- Take advantage of employee assistance programs (EAPs) if available.
- Advocate for systemic change in your organization to make mental health resources more accessible.
Getting help early can prevent more severe burnout and keep workers engaged in their careers.
The Role of Organizations in Supporting Self-Care
While individual self-care is crucial, the responsibility does not fall on workers alone. Healthcare systems must also create environments that support staff well-being. This can include:
- Adequate staffing levels to prevent chronic overwork.
- Mental health resources that are confidential and easily accessible.
- Fair scheduling practices that allow for recovery time.
- Recognition programs to show staff that their contributions are valued.
When organizations support their workforce, they see lower turnover, better patient outcomes, and improved morale.
Conclusion
Self-care is not a luxury for healthcare workers—it is an ethical and professional responsibility. By taking steps to prioritize their own well-being, clinicians can continue to provide high-quality care without sacrificing their health in the process.
Healthcare is a demanding field, but with consistent, intentional self-care practices and organizational support, it’s possible to build a career that is both sustainable and fulfilling.